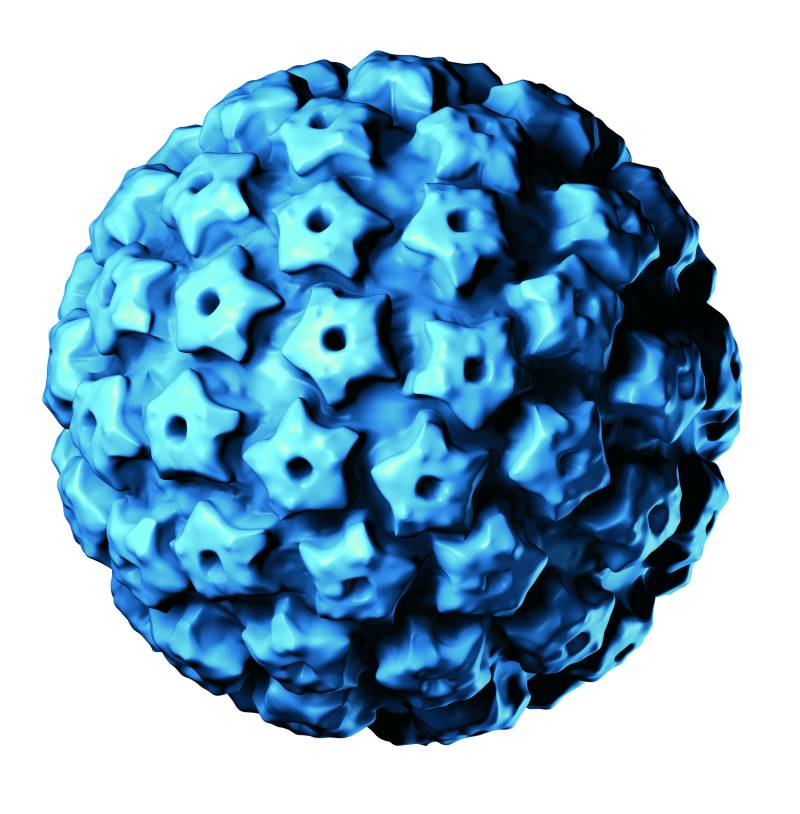
Results from a new study suggest that the human papillomavirus (HPV) vaccine is effective in preventing the development of several types of cancers caused by HPV, most particularly head and neck cancer in males.
The research will be presented at the 2024 American Society of Clinical Oncology (ASCO) Annual Meeting, taking place May 31-June 4 in Chicago, Illinois.
About the Study
“This study adds to a growing body of evidence demonstrating decreased rates of HPV-related cancer among people who received the HPV vaccination. The CDC reported that in 2022, less than 60% of children ages 15-17 had been vaccinated for HPV, suggesting that a large portion of the population is more vulnerable to HPV infection and, in turn, more vulnerable to the development of HPV-related cancers. Identifying effective interventions that increase HPV-vaccination rates is critical in reducing undue cancer burden in the United States,” said lead study author Jefferson DeKloe, Research Fellow, Thomas Jefferson University.
Previous research pertaining to HPV-vaccination has primarily focused on outcomes related to cervical cancer. It is the fourth most common cancer globally with about 660,000 new cases diagnosed annually with nearly 350,000 deaths per the World Health Organization. This study examines the HPV-vaccinated persons’ risk of developing cancers of the head and neck, anal areas, penis, vulva, vagina, and cervix. This study also aims to examine the HPV vaccine’s impact on need for surgical treatment of cancer and pre-cancerous lesions.
This study included 1,706,539 patients vaccinated for HPV and 1,706,538 age-matched control patients with no prior HPV-vaccination. A total of 56% were female, 53% were White, 21% were Black/African American, 5% were Asian, 0.4% were American Indian or Alaskan Native, 0.4%were Native Hawaiian or Other Pacific Islander, and 21% were of other or unknown race.
“We have known the HPV vaccine decreases rates of oral HPV infection, but this study shows that in boys and men in particular, vaccination decreases the risk of HPV-related oropharyngeal head and neck cancers. HPV vaccination is cancer prevention.” – Glenn J. Hanna, MD, Director, Center for Cancer Therapeutic Innovation, Center for Head and Neck Oncology at the Dana-Farber Cancer institute.
Key Findings
- Males vaccinated for HPV had a lower risk of developing all HPV-related cancers (3.4 cases per 100,000 vaccinated patients vs. 7.5 per 100,000 unvaccinated patients), as well as a lower risk of developing head and neck cancers compared to unvaccinated males (2.8 cases per 100,000 vaccinated patients vs. 6.3 per 100,000 unvaccinated patients)
- Females vaccinated for HPV had a lower risk of developing cervical cancer (7.4 cases per 100,000 vaccinated patients vs. 10.4 per 100,000 unvaccinated patients) and a lower risk of developing all HPV-related cancers compared to unvaccinated females (11.5 cases per 100,000 vaccinated patients vs. 15.8 per 100,000 unvaccinated patients). However, odds of developing head and neck cancers and vulvar or vaginal cancer were not significantly different in vaccinated females compared to those who had not received the vaccine.
- Vaccinated females without a prior diagnosis of abnormal findings during a Pap test were less likely to develop precancerous dysplasia of the cervix and undergo invasive procedures to treat and prevent precancerous lesions.
Next Steps
Next steps will include examining outcomes in HPV-vaccinated people older than 39 years of age now that some form of the HPV vaccine has been available for nearly two decades. The investigators hope to look at outcomes based on age at time of vaccination, time from vaccination to development of cancer among people who do develop cancer, and discerning which populations are less likely to undergo HPV vaccination.
This study received no external funding.
